Posts Tagged ‘advocacy’
Musing Together: Looking at Art Expands Skills, Increases Socialization, and Widens Horizons
 The group pauses in front of a large contemporary sculpture, depicting a preacher standing before his congregation at a small country church. They walk around the piece, noticing the pews, the organist, and the variety of parishioners, and chatting as they view. Then they settle into chairs and co-facilitator Esther Smith asks: “What is one word that comes to mind when you look at this piece of art.”
The group pauses in front of a large contemporary sculpture, depicting a preacher standing before his congregation at a small country church. They walk around the piece, noticing the pews, the organist, and the variety of parishioners, and chatting as they view. Then they settle into chairs and co-facilitator Esther Smith asks: “What is one word that comes to mind when you look at this piece of art.”
“Boring,’ says one woman.
“What makes it boring?” Esther asks.
“It brings me back to my childhood, when I was stuck in church for hours,” she answers. “I was so bored.”
A few others nod. Someone asks, “When was this made? Where is it from?” and the conversation about the art continues.
Every month at the High Museum in Atlanta, Georgia, Teaching Artist Esther Smith guides a group of care partners and people living with dementia on a 90-minute gallery exploration called Musings Together.
“It’s a light-hearted, interactive experience,” Esther says. “We go at a slow pace, seeing only three to four works each time. We want people to have a comfortable, personalized experience with art.”
 The open-ended conversation brings out people’s stories and ideas. Sitting in front of Giovanni Bellini’s Madona and Child, Esther asks, “What lines do you notice in this painting? Trace them in the air with your hand.”
The open-ended conversation brings out people’s stories and ideas. Sitting in front of Giovanni Bellini’s Madona and Child, Esther asks, “What lines do you notice in this painting? Trace them in the air with your hand.”
After people trace their lines, she asks, “What line was most interesting to you?” That question might lead into a discussion of what makes this painting different. Then Esther might invite the group to pose like the picture. She might say, “How would that baby’s head feel in your hand?”
“These simple prompts launch us into deep conversations,” Esther says. She and her team are experimenting with expanding the sensory experience, including bringing out oranges when they’re gazing at a still life of fruit and letting each guest hold and examine the orange. Esther also invites people to occasionally sketch an aspect of a drawing that appeals to them, using a drawing pad on a clipboard.
“ A number of our participants have never been regular museum-goers. Now they feel comfortable here and come more often,” Esther says. “Developing a new community of friends and an expanding interest in art enriches their lives.” #
Want to look at art with someone who is living with dementia?
If you’re visiting a museum, focus on a gallery with 3-4 large and interesting pieces. Ask a docent for advice, if needed. If you’re at home, give yourself plenty to time to comfortably view a few works of art on-line or in books.
- Bring a folding chair, so you can sit.
- Chose a time of day when your partner is energetic and the gallery is relatively quiet.
- Have fun just noticing the aspects of the piece. You might invite comments on colors, textures, familiar figures, objects that seem odd to you, and other aspects.
- Ask open-ended questions, such as, “What does this piece make you think of?” “What do you like about this piece?” “How do you think that main guy feels?”
When attention wanes, move onto something else, including a lovely coffee or tea break.
Click to view informative and inspiring short videos on our YouTube channel
Deborah Shouse is the author of Connecting in the Land of Dementia: Creative Activities to Explore Together and Love in the Land of Dementia: Finding Hope in the Caregiver’s Journey.
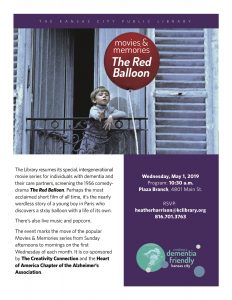
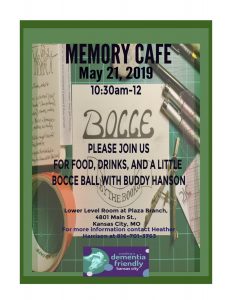
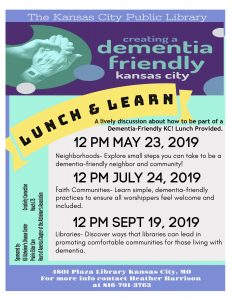
Free events for people living with dementia and their care partners
What They Don’t tell You About Dementia: A Guest Post by Laurie Scherrer
Laurie Scherrer is a light in the universe. I met her on the radio, when she co-hosted the ground-breaking program Alzheimer’s Speaks, with Lori La Bey. I was instantly inspired by Laurie’s warmth, honesty, humor, and insights. Each time I talk to her, I have fun and I learn from her. Recently, I asked her, “How can I support you in the wonderful advocacy work you are doing?” Laurie answered, “You can repost this blog, What They Don’t Tell You about Dementia.”
Laurie’s post is not just inspiring: it could be life-changing for someone who is newly diagnosed with dementia. After reading it, you’ll want to subscribe to Laurie’s blog.
What They Don’t tell You About Dementia: by Laurie Scherrer, DementiaDaze.com
When I was diagnosed with dementia (Early On-Set Alzheimer’s and Frontotemporal Degeneration) the doctors told me and my husband:
- My working days were over
- I needed to “Get my affairs in order and see an attorney”
- The time would come when I wouldn’t recognize my loved ones
- For any additional information we should go to the Alzheimer’s Association Website
- I may experience “sun-downing” in the late afternoons
- Come back in six months to see how rapidly you have progressed
 What the doctors SHOULD have told us:
What the doctors SHOULD have told us:
- There are many things that can aggravate or enhance the confusion and agitation that comes with dementia. With observation and patience, you may be able to recognize what triggers these symptoms. For example noise, stress, over-stimulation or lack of sleep. These triggers are not the same for everyone.
- Once you recognize the triggers you may be able to find ways to lessen their impact. For example, use earplugs when in a store or restaurant to reduce the noise, keep gatherings small to avoid over-stimulation, and when needed take an afternoon nap.
- The more independence you give up and allow other people to take care of – the more dependent you will become on others. Change your thought process from “I can’t do this anymore” to “How can I accomplish this task (what changes or modifications can we make to assist me).”
- On days when you are using a lot of cognitive reserve your symptoms may be strong (usually in the afternoon). This is your brain saying it is tired and needs a break. Try listening to some music or taking a nap.
- It is OK to take some time to grieve for your losses and accept that life will change. Most people need to experience this after diagnosis and again as their abilities change. In addition to grief, you may experience shock, anger, denial and sadness. These are normal reactions that can help you come to terms with your disease and hopefully help you to move on.
- Get involved with others with dementia as much as possible. There are a number of groups that offer video chats with other people living with dementia so you can socialize, ask questions and encourage each other. dementiamentors.org offers a mentor program so you can have weekly chats with someone living with dementia.
- Stay active and socialize with old friends and new. Once you curl up into yourself it is hard to get out. Enjoy life, friends, family and activities for as long as you can.
- Build your passion to fight back! Sometimes it is the passion within us that drives us to continue fighting. Get involved in advocacy work to educate about dementia. Contact Dementia Action Alliance at daanow.org to get started.
- You will have good moments when you feel “normal” and think you should go back to work and you will have bad moments when the world is a fog (dementia daze zone). You may feel confused and disoriented and find it difficult to think. There will be times when nothing seems to make sense and you can’t remember how to do things and then the fog will go away (at least for awhile). It’s OK to admit you are having a bad day.
- Dementia is more than memory loss. You may experience problems with your balance, lights flickering in your eyes, hallucinations, develop fears, or smell things that aren’t really there. Don’t be frightened, keep track of any changes or strange feelings to see how often they occur
- Dementia can progress fast, but in most cases it is a long slow progression. You may want to keep your affairs in order, but by implementing changes and strategies you will be able to overcome many obstacles and live a beneficial and happy life for some time.
Since I’m sure your doctor said about the same thing as mine, I hope you find this helpful. Now go enjoy life – Live, Love and figure out how to make adjustments to over come your obstacles.
My motto is: I don’t want just to survive – – I want to live and thrive!

Love & Laughter,
Laurie

Educating on Dementia: A Vietnamese Doctor’s Quest
Throughout our journey in Vietnam, we met a number of inspiring elders. These include an 87-year-old public letter writer in the old Saigon train station, a 67-year-old woman carrying baskets of pomelos and bitter melons, a beautiful 74-year-old gardener hacking at weeds with a machete, a 100-year-old matriarch in a farming family, and an 83-year-old village chief. Because the life expectancy in Vietnam has risen over the last 20 years, its people are living longer. Along with that blessing comes an increased chance of dementia. Neurologist Trần Công Thắng. MD, and his team, Nguyen Tudny Vy and Le Thi Yen Vy, are dedicated to working with medical professionals and community members, educating on dementia.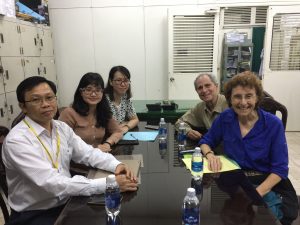
“Many people think memory loss is just part of normal aging, ” Dr. Thang told us, when we visited him in Choray Hospital in Saigon. “We want people to understand that dementia is not a regular part of growing older—it’s a brain disease.”
Twenty years ago, few people were discussing dementia in Vietnam. But now, it’s a vital issue for two reasons. First, the country’s life expectancy has increased from age 64 to age 75. Second, many families no longer have seven or more children; they have two to three offspring. This intensifies the burden for family caregivers.
 Dr. Thang is a researcher, speaker, educator, and a founding member of the Association of Vietnamese Alzheimer’s Disease and Neurocognitive Disorders. Through his classes and diagnostic clinics, Dr. Thang and his colleagues offer people much needed information and resources. He is partnering with a local rehabilitation hospital in creating a day program for those living with dementia. The program will offer cognitive stimulation and social engagement for those living with dementia.
Dr. Thang is a researcher, speaker, educator, and a founding member of the Association of Vietnamese Alzheimer’s Disease and Neurocognitive Disorders. Through his classes and diagnostic clinics, Dr. Thang and his colleagues offer people much needed information and resources. He is partnering with a local rehabilitation hospital in creating a day program for those living with dementia. The program will offer cognitive stimulation and social engagement for those living with dementia.
Person by person, Dr. Thang is helping healthcare professionals understand the behaviors and issues associated with dementia. He hopes to make life better for family caregivers and their family members who have memory loss.

“Stamp” out Alzheimer’s
 Do your part to “Stamp our Alzheimer’s.” For twelve years Lynda Everman was a silent caregiver. Her husband, Richard, was diagnosed with Mild Cognitive Impairment in 1997; in an effort to preserve his dignity, she told few people what they were going through.“We were both introverts and private people,” Lynda says. “My husband and I were a team, taking care of each other, moving through a situation that was too painful to address in public.”
Do your part to “Stamp our Alzheimer’s.” For twelve years Lynda Everman was a silent caregiver. Her husband, Richard, was diagnosed with Mild Cognitive Impairment in 1997; in an effort to preserve his dignity, she told few people what they were going through.“We were both introverts and private people,” Lynda says. “My husband and I were a team, taking care of each other, moving through a situation that was too painful to address in public.”Here’s where you come in.
Ten More Steps to Make Your Community Dementia-Friendly
I’ve been thinking about Michelle’s ideas, inviting us all to be part of creating a more-dementia friendly community. Here are additional thoughts from Michelle Niedens, L.S.C.S.W. Director of Education, Programs and Public Policy, at the Alzheimer’s Association’s Heart of America Chapter.
What volunteers would walk with their neighbors who were living with Alzheimer’s disease, so they could exercise and visit with others, without worrying about getting lost?
What if neighbors volunteered to visit regularly or run an errand?
What if law enforcement went beyond Silver Alerts and had standardized protocol for individuals who wander and go missing?
What if gas stations and convenience stores had training to recognize someone who might be lost?
What if pharmacies provided support information any time an Alzheimer’s drug was prescribed?
What if doctor’s offices had “memory aware” time slots, so people living with dementia wouldn’t have to wait in a noisy, chaotic environment?
What if there were geriatric urgent care settings?
What if grocery stores had a “slow down” line?
What if grocery stores had designated times when shopping support was available?
What would it take for all of us to be “memory aware” and to act on that?
……………………..
I want to do something to help here in Kansas City, but I haven’t yet decided what. In my upcoming book, Staying Connected in the Land of Dementia, I write about Meet Me at the Movies & Make Memories, a movie-going event for those living with dementia and their partners, co-created by John Zeisel. That really appeals to me and I’m thinking about contacting local theater owners. I welcome collaborators and I also would love to hear your ideas. What actions are you inspired to take?
Deborah Shouse is the author of Love in the Land of Dementia: Finding Hope in the Caregiver’s Journey.
Eight Paths towards a More Dementia-Friendly Community
On November 10, 2015, Michelle Niedens, L.S.C.S.W. Director of Education, Programs and Public Policy, at the Alzheimer’s Association’s Heart of America Chapter, gave a beautiful talk, inviting all of us to contribute to a compassionate, inclusive, and dementia-friendly community. Her ideas are both simple and profound and offer a challenge and an invitation for all of us. Over the next two weeks, I’m going to share some of Michelle’s visionary “what if” thinking.
From Michelle:
What would it take for all of us to be memory aware and to act on that?
What if restaurants had finger food menus? What if restaurants had specials from the finger food menu in the middle of the afternoon, when there were fewer people in the restaurant and things were quieter?
What if theatres had showings designed “memory aware”?
What if theatres had showings of old movies monthly with the “memory aware” icon on the website, so families could still enjoy getting out and having the cinema experience?
What if radio stations played songs related to memory issues in November (Alzheimer’s month) or April (Caregiver month)?
What if retail stores had designated days when the staff wore “memory aware” name badges and could provide more support to shoppers?
What if technology-based stores had annual displays of products that support memory, safety, or organization?
What if faith communities identified in bulletins/newsletters those activities that were “memory aware?”
Deborah Shouse is the author of Love in the Land of Dementia: Finding Hope in the Caregiver’s Journey.
Four Reasons You’ll Want to Read This Book
The thoughts creep in, quietly, sneakily, like Sandburg’s fog “on little cat feet.” I walk into the living room and puzzlement seizes me. I ask myself, “Now why am I here?” I am writing to my cousin and suddenly can’t remember his life partner’s last name. And then there’s the mysterious case of the forest green shirt in the night, gone missing now for four and a half weeks.
Perhaps you, too, deal with these flash thoughts: “Am I feeling the first confusions of the deeply forgetful?” (That’s the beautiful way Stephen G. Post, PhD, refers to memory loss.)
“If I should become more deeply forgetful, I want to be sure you read this book,” I tell Ron.
“This book” is I’m Still Here by John Zeisel, PhD, and I felt enveloped with grace, compassion, and excitement while I was reading it. John is the president and cofounder of Hearthstone Alzheimer Care, and a writer, professor, and vigilant advocate for those living with dementia.
He writes about how he’s been transformed by working with people living with dementia. He orchestrates care partner conversations, where they discuss the gifts of being present for their loved ones with dementia. He’s brimming with creative ideas and activities that bring life and fun to care partners.
With his colleague, Sean Caulfield, he drew into existence the Meet Me at MOMA arts program for those living with dementia, and now offers a variety of artistic and creative programs all over the world. He’s involved in a number of other innovative programs through his foundation, including It Takes a Village, designed to keep people living with dementia connected to their communities and to themselves.
Here is one of John’s thoughts that really speaks to me: “Everyone has his own unique capabilities. … It is our job to uncover, celebrate, and embrace these abilities, so everyone living with Alzheimer’s maintains dignity, independence, and self respect.”
Those words are easily just as true if they read: “Everyone has his own unique capabilities. … It is our job to uncover, celebrate, and embrace these abilities, so everyone maintains dignity, independence, and self respect.”
If you want to feel more connected to someone who’s living with dementia, if you want to celebrate yourself as a care partner, if you want to understand more about the dementia experience, if you want a dash of inspiration and a long cool drink of hope, you’ll love reading this book.
To Learn More about The I’m Still Here Foundation’s programs, visit www.ImStillHere.org
To Learn More about Hearthstone Alzheimer Care, visit www.TheHearth.org
To learn more about John, just Google his name
To order John’s book, visit Amazon.com or another online bookstore
Deborah Shouse is the author of Love in the Land of Dementia: Finding Hope in the Caregiver’s Journey.
Returning to Who He Was: Richard Taylor’s Journey as an Advocate
“Dementia has brought me back to who I was to begin with. I’m more self confident in myself. I feel an intensity in the moment that I didn’t have before.” Richard Taylor, PhD.
 Living the Before and After: From Professor to Unemployed to Author and Speaker
Living the Before and After: From Professor to Unemployed to Author and Speaker
Before he was diagnosed with dementia, Richard was a professor of psychology. At age 62, he was a popular lecturer, witty, well read, with an easy manner and a welcoming charm. But when he was diagnosed with dementia, Richard lost his professional standing, his job, his driver’s license, his confidence, and his optimism. He found himself crying ceaselessly, not really understanding why.
“I didn’t even know anything about dementia,” Richard says. “I had fears about losing control of myself. I thought the transition from one stage to another was abrupt, that a curtain would drop and suddenly I wouldn’t know the world and the world wouldn’t know me.”
To stem these fears, Richard began to write daily, capturing these thoughts and activities: he was, after all, a psychologist and used to analyzing things. Every morning, he read his previous day’s writings.
After he had accumulated a year’s worth of writing, he read some excerpts to the members of his Early Onset support group.
His group identified with his fears and feelings and urged him to take his pages down to the caregiver’s support room and slide them under the door. Richard did.
After both meetings ended, some of the care partners sought out Richard to thank him for sharing his feelings and insights. Months later, someone from Health Professionals Press called and asked if they could publish Richard’s writings. His book was titled Alzheimer’s from the Inside Out.
Turning into an Advocate and Speaker
“Since I’d written a book, people thought I seemed smart and interesting,” Richards says. 
He was invited to read parts of the book.
“My introductions to my readings got longer and longer,” Richard says. “I wanted to share my dementia story, so I talked about my life and what it felt like. I’ve always felt people with dementia are the only true experts on the subject. You can imagine you’re blind, but you can’t imagine you have dementia. Dementia is so individualized as to how each person expresses it. Our brains each have different strategies.”
Soon people were paying Richard to share his insights at conferences and conventions and his speaking career began.
He starts his presentations by saying, “My name is Richard and I am living with the symptoms of dementia.”
But Richard didn’t confine his advocacy to speaking. He also worked with the Houston Art Museum and the Metropolitan Museum of Modern Art to bring an art program for people with dementia to the gallery. Richard traveled to MOMA, learned about the program, worked with the Houston docents, and was a catalyst for bringing the program to the Houston community.
Understanding the Loss and Lack of Meaning
Imagine losing your job, your car and your sense of passion and purpose. You feel you’ll never again do the activities you love, make new friends or try new hobbies. Your life is static and boring and you feel out of place and alienated, even in your own home.
Richard believes many with dementia prematurely talk themselves into a wheelchair and into not communicating. They give up. He understands the loneliness and despair that can overtake someone living with dementia.
“Strangers start hugging and kissing you and talk louder to you and never ask for your opinion and are more effusive in their positive emotions with you. After a while, you just go along. So when people say, ‘How are you doing honey?’ I say, ‘I’m doing fine.’”
Reigniting His Purpose
Richard hopes his personal stories will inspire care partners to look for opportunities to bring more joy, connection, and satisfaction into life. He understands how important it is to feel a sense of purpose. As a debater, a professor, and a raconteur, Richard has always defined himself through his speaking and writing.
“Through my speaking and advocacy, I have reignited my sense of meaning,” Richard says. “People clap when I talk and this reassures me.”
Part of Richard’s purpose is helping care partners see their loved ones as whole and complete. He writes, “Just because my memory sometimes fails me, just because my cognitive abilities seem to slip…please know that in my own heart and mind, I am still me. I am not becoming any less a person simply because I cannot remember like you, talk like you do, or think as you do. I am still Grandpa, and Dad, a friend.”
Richard believes, “Dementia is about living a purposeful and purpose-filled life, not dying from its causes.”
Creative Sparks:
When talking with someone who has dementia, Richard has this advice:
- When greeting someone who has dementia, say, “Hello, it’s me, Deborah.” Then pause, allowing time for a response.
- If you don’t know how to act or what to say when you’re visiting a friend with dementia, try to learn more about what your friend is experiencing. You might ask, “What have you learned from living with dementia?” Or, “What changes are you having to cope with?” Or, “How can I make our time together more meaningful?
- See the person as a whole human being.
- Look for opportunities to add autonomy, purpose, and adventure to the person’s life.
Thanks to Richard Taylor for sharing his wisdom. Richard passed away from cancer on July 25, 2015, but his spirit and his advocacy work will long live on.
Thanks to Lori La Bey for sharing my article about Richard with her readers.
Please visit her site https://www.alzheimersspeaks.com
for more information about Richard, including an interview with Lori.
Lori’s site, blog, and radio program feature inspiring people who are working for and with those living with dementia.
Deborah Shouse is the author of Love in the Land of Dementia: Finding Hope in the Caregiver’s Journey.
Inside Advocacy with Karen Love: Making a Difference for Those Living with Alzheimer’s
Alzheimer’s is a democratic disease and no one is immune. Movie stars, politicians, bankers, comedians, business moguls, professors, and homemakers– any one of us could face living with dementia. Karen Love is a founder of the Dementia Action Alliance, which focuses on improving dementia care for the more than five million Americans currently living with the condition. Karen works with governmental agencies to define and improve a person-centered standard of care for elders and for those living with dementia. She’s an inspiring leader and I wanted to share some of her insights with you.
Q and A
Q: What prompted you to form a non-profit and become an advocate for aging and for those living with dementia?
A: Advocacy must be in my DNA. Even as a girl, I was always sticking up for people and their rights. I initially worked as an administrator in assisted living and I became concerned about how fast the industry was growing without paying attention to the needs of its vulnerable residents, particularly those who had dementia. In 1996, I founded a non-profit organization, Consumer Consortium for Assisted Living (CCAL), to advocate for, support and educate consumers about assisted living. After a decade, we renamed the organization CCAL—Advancing Person-Centered Living, and we expanded our mission to encompass all elder care settings. We focused on promoting quality of life and person-centered practices.
Q: You’ve worked with Medicaid and Medicare to help define and implement a mind-set of person-centered care. What does person-centered care mean and why is it so important?
A: The World Health Organization and the Institute on Medicine recognize Person-Centered practices as the gold standard. Person-centered practices support people’s emotional, social, physical, and spiritual well being. They focus on treating people with dignity, fostering choice, independence, and feelings of purpose, value, and self-worth. These practices also help people maintain normalcy in their daily life. I’ve had the honor to help shape the person-centered framework for CMS’s home and community-based division, which support such state-based services as home care, adult day, and assisted living for individuals Medicaid eligible.
Q: You’ve now gathered thought leaders in the fields of aging and dementia, building a coalition of people dedicated to “making dementia better” in our country. What are some of your goals?
A: Our goals include:
- Enhance knowledge about dementia and person-centered care practices so people living with dementia are no longer stigmatized.
- Improve healthcare practitioners’ understanding and knowledge about dementia care, person-centered practices and treatment, and make sure materials are accessible.
- Share information with care partners and healthcare providers about the value of attending to emotional, social, and spiritual well being.
- Increase federal and state funding for dementia-care related support.
Q: What are some inspiring actions that ordinary caregivers or persons living with dementia have taken?
A: Just a couple of examples include:
- Michael Ellenbogen is a person who is living with dementia. Prior to being diagnosed, he was a high-level bank executive. He has become a tireless advocate and spokesperson for dementia.
- Lori La Bey started an online weekly radio program called “Alzheimer’s Speaks” to provide a venue for people to learn about dementia, share their experiences, and be supportive.
Q: What are three easy things each person can do to act as an advocate for those living with dementia?
A: Here are some suggestions:
- There are three ways things change nationally: (1) the President makes it happen (2) Congress makes it happen (3) the groundswell of people’s voices and actions make it happen. There has not been an interest for the first two methods. Historically, method 3 was effective for impacting and changing issues such as HIV/AIDS and breast cancer. The Dementia Action Alliance brings people together so we can be a catalyst for change.
- Words matter. Often people living with dementia, including Alzheimer’s, are called “patient,” “victim,” “demented,” and “sufferer” – and the condition is called a “dementing illness” and an “affliction.” This type of language can impact how people living with dementia feel about themselves and how they are treated by others. Print out “Use Words Wisely” from the website – www.daanow.org/words-matter/- and help educate others about what words to use.
- Email the Dementia Action Alliance at info@daanow.org about your interest in volunteering. Consider making a financial donation at www.daanow.org The more people involved in the Dementia Action Alliance, the sooner and greater the impact.
Please feel free to share this information with your friends and colleagues. The more we all work together, the more effective our voices will be.
Deborah Shouse is the author of Love in the Land of Dementia: Finding Hope in the Caregiver’s Journey.